Jonathan Conta is a product management and product marketing leader with extensive expertise in the medical devices space. He was most recently Vice President of Product Management at Intuitive, a technology company focused on minimally invasive care and robotic-assisted surgery. Jonathan began his career in research at Beth Israel Deaconess Medical Center before pursuing an MBA at the Kellogg School of Management. From there, Jonathan moved into planning and development, and, later, marketing management at CR Bard, a medical equipment manufacturing company, before joining Intuitive.

In our conversation, Jonathan shares experiences heading up teams that transform modern surgery by leveraging robotic assistance to improve patient outcomes. He discusses the nuances of disrupting such a high-risk, regulated industry, as well as the adoption paradigms that come with that. Jonathan also offers insights from overseeing medical training programs and discusses how he’s transferred those into his own mentoring practices.
I see it as disrupting how a surgeon approaches a particular patient. In the past, when evaluating patients with difficult anatomy or advanced cancers, the surgeon would likely say, “I need to open this patient up and make a large incision where I can insert my hands and see, under direct visualization, exactly what’s going on.”
Robotic surgery disrupts that thought process and uses technology to perform minimally invasive surgery on the same patient. It brings a lot of benefits to the patient’s health and recovery, such as small incisions, minimal blood loss, reduced complications, low risk of readmission, and more.
The paradigm that I indirectly witnessed was the shift in prostatectomy, or the removal of the male prostate gland. This is a very common surgery all over the world and, prior to robotics, was predominantly performed via “open” surgery — this involves a large incision where the surgeon places their hands and tools directly inside the patient. However, over time surgeons have found great success in utilizing robotic assistance to not only make that procedure minimally invasive but also extract additional benefits — like nerve sparing — through the visualization and precision of robotics.
With an open surgery, men often find that they are impotent or incontinent after a radical prostatectomy. The insertion of robotics into this procedure has dramatically reduced this risk. We can take that shift in paradigm and then say, “All right, what other procedures could benefit from this technology that looks similar to prostatectomy?” I helped usher a move toward using this technology in applications benefitting women’s health — looking at uterine and cervical cancers — to bring the same benefits that men saw for prostatectomy to women.
There was resistance from all of those groups in different ways. For surgeons, this was a new tool. It’s not something the majority were exposed to in their residency or training programs. Some will say, “Where am I going to find the time to learn this safely and integrate it into my practice?” Others might say, “I don’t need robotics. I’m a highly skilled surgeon — this is a crutch.”
In the early days of robotic surgery adoption, insurance companies looked at this technology at first as an expensive toy, and as a result, wouldn’t sign off on it until they had seen proven results. That took years. Patients, interestingly enough, experienced a social bifurcation. Men looked at robotic technology and said, “Sure, I’m willing to have a surgeon use this robot to operate on me.” Women were much more reticent about that. Those social dynamics, at least in the United States, resulted in differing adoption speeds among those patients.
There are processes that the FDA and other notified bodies around the world use to ensure certain levels of safety. In the United States, we have a 510(k) process, which is designed to establish substantial equivalence. In other words, an evaluation will be done to compare this new device with something that’s already been cleared.
Once it gets out into the market, however, the bar by which surgeons measure that is, in many ways, much higher. First is safety — let’s prove that the use of this technology does no harm, and, if nothing else, lowers the percentage of patients that would see a detrimental outcome. Once we’ve proven safety, we need to prove efficacy. We have to demonstrate that the outcomes for the patient are superior, and that starts with a single surgeon in a single center presenting their experience.
Then it moves to multi-centers and multiple surgeons looking retrospectively. They look backward at what they used to do before robotics and compare it to what they do now with robotics. After that, we start looking prospectively. This is when surgeons say, “I’m now going to start at time zero and I’m going to compare robotics to whatever I would have done otherwise. I’m going to either randomize the patients as to who received which type of surgery, or I’m going to match them based on certain characteristics to make the groups comparable.”
Finding surgeons who are willing to undergo this substantial effort is also a challenge. That’s where the art of marketing lies — finding the right personalities and institutions that are interested in thinking forward. They want to remove their own biases and look at things with a clean set of eyes. That’s what I find the most fascinating about this work — it’s so fun and inspiring to work alongside these brilliant people who are giving care while trying to push the envelope and raise the bar at the same time.
Absolutely. The business value from the hospital perspective is twofold. Efficiency is a very important one, as there is always a learning curve. It’s going to take time for the surgeon to gain proficiency, as well as for care teams within the operating room to gain efficiency as well. Any robotic system requires setup and takedown time, so that has to be incorporated into the efficiency calculations. But the evidence shows that if hospitals look at robotics in terms of the total cost to treat a patient, the reduced complications and length of stay that robotics enables can actually have very positive financial effects.
The second part is overall profitability. If a hospital makes a multi-million-dollar investment in robotics, they’re going to want to see a return. This is measured in a few ways. One is decreasing the time patients spend in the hospital, especially where robotics enables the patients to recover faster and, therefore, go home faster. That is a cost avoidance that accounting departments can easily track. Another is the number of procedures done robotically. The robot can’t sit in an operating room and only be used once a week by one surgeon, which is why having multiple clearances for multiple types of pathologies helps with this ROI.
Regulation is a constant force in the medical device world and anything that has to do with healthcare. The safe and responsible adoption of technology is a burden both on the industry side, as well as the caregiving side. The two have to work together to prove the safety and efficacy of these devices.
The partnership has to present a unified front to the regulated body and ask for permission to look at a set of procedures or specialties. The goal is to establish the unassailable fact that the use of this technology creates better outcomes for patients. With that, the FDA, hospitals, and manufacturers need to work together to lay out what each stakeholder cares about and what it means for them. Often, there’s a lot of common ground. Doing this process safely and responsibly is the most important thing, and that requires a partnership.
Most initiatives start with a limited launch scenario where you bring the new technology to known partners — people you have worked with before — who are highly experienced in using the technology. They can pick up on the subtleties of what they used to do versus what they are now going to do with the new technology.
The responsible thing is to start with a small group of experienced users, put the device in their hands, and say, “Is it working the way you expected it to? Is it extracting the additional benefits that we all hoped that it would? Are we seeing the intended results and the outcomes that the technology was purposed for?”
Once that limited launch has gone forward, we can start with a phased and broader rollout. The important feedback loops involve the surgeon and the commercial teams. The commercial teams are the product team’s initial point of contact. This is one or more people, sitting next to that surgeon in the operating room for a number of those first cases, who then translate that feedback back to the product development teams. This ensures that we’re being honest and accurate in how we portray what happened in the operating room.
It’s sometimes hard for product management folks to be intellectually honest about how the first few cases went because they feel personally invested in the product they’ve spent years developing. This feedback loop ensures that everyone is rigid and accurate in telling the development teams how the product is actually performing in the hands of users.
Taking copious notes amid the procedure, while also being very factual about it, is incredibly important. When considering the key objective measurements of the launch, I think back to an impactful book I read a while ago called Measure What Matters. Are we looking at this through the right lens? Are we defining the right KPIs and measuring the right thing? Sales is one measurement, sure. It’s certainly a good one from a top-line revenue standpoint, but maybe it’s not the best measurement of whether we hit the mark in terms of meeting user needs.
The design of training programs is done in combination with several teams. The product management team works with training teams, which work with clinical affairs and other departments. My prior company, Intuitive, has an entire department that is involved in the professional education of surgeons. This means asking questions like:
Next, you have to consider how much needs to change in the surgery process. If the training can be done on an animal or dry model, then that’s not a huge lift, but if it needs the fidelity of a cadaver model, that’s more expensive and involved. All of this will affect the rollout. They’re all interconnected, so you have to be careful and purposeful in terms of how you think about them.
This is where partnering with experts in instructional design is incredibly important. Product management will come to them and say, “Here are the three things that we think we need to impart upon the surgeon for them to safely adopt this technology.” Instructional design will say, “All right. Based on that, this is how we create modules, online training, and hands-on learning.”
Absolutely. The old adage in medical training is: see one, do one, teach one. That’s totally unsafe and unrealistic in our world. We’ve learned a lot in a couple of generations since that became a moniker, but I apply other concepts in my own mentorship, like thinking in terms of one-way doors and two-way doors. Two-way doors say, “If you make a mistake, we can back this up and try again, and we can learn from that.” One-way doors do not allow backing up.
For example, there are moments in surgery where you need to cut a vessel. Once you’ve cut that vessel, it’s nearly impossible to go back. That’s a one-way door. The same idea applies to mentorship. Two-way doors let people develop and give them the opportunities to make mistakes. It’s straightforward to then go back and undo that mistake.
One-way doors should be a two-person conversation. Allow the mentee to present the data which supports that recommendation. Then, if the mentor decides that’s probably not the right idea or the right decision, you have to teach them and explain that this would’ve been a one-way door. Let’s back up and figure out how we got to this assumption, and we can correct this thinking for next time. Overall, people learn much more from mistakes than from successes.
I think the biggest element is self-awareness. Everyone brings strengths and weaknesses to a particular job. Their passion and interest might not perfectly align with what they’re good at. That’s where coaching has to come in to say, “Listen, I strongly believe that turning your weaknesses into strengths is probably a fool’s errand. Let’s take your strengths and make them superpowers, and let’s do what we can to minimize your weaknesses.” It takes a significant amount of self-awareness for someone to recognize their strengths and weaknesses, and a big part of mentorship is helping that person figure out those qualities.
Often our spouses and co-workers know us better than we know ourselves on several levels, so being open enough to accept feedback is critical to gaining better self-awareness. When an employee wants to head in one direction, as a mentor, you should give them opportunities to do that. At the same time, you should point out where their strengths lie and encourage them to play to those strengths. That is going to help them advance in an organization that much faster.
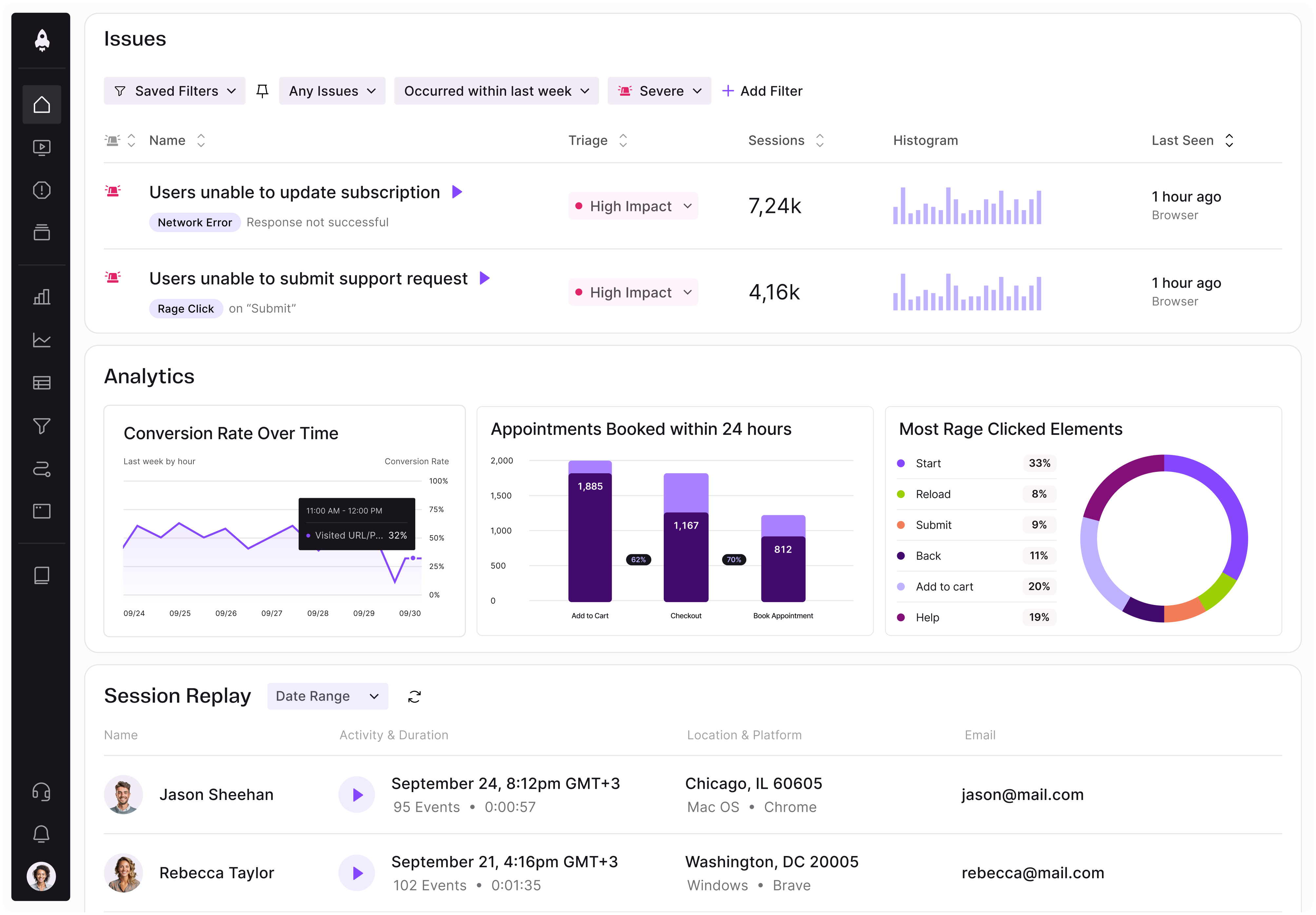
LogRocket identifies friction points in the user experience so you can make informed decisions about product and design changes that must happen to hit your goals.
With LogRocket, you can understand the scope of the issues affecting your product and prioritize the changes that need to be made. LogRocket simplifies workflows by allowing Engineering, Product, UX, and Design teams to work from the same data as you, eliminating any confusion about what needs to be done.
Get your teams on the same page — try LogRocket today.

Rahul Chaudhari covers Amazon’s “customer backwards” approach and how he used it to unlock $500M of value via a homepage redesign.
A practical guide for PMs on using session replay safely. Learn what data to capture, how to mask PII, and balance UX insight with trust.

Maryam Ashoori, VP of Product and Engineering at IBM’s Watsonx platform, talks about the messy reality of enterprise AI deployment.
A product manager’s guide to deciding when automation is enough, when AI adds value, and how to make the tradeoffs intentionally.