Nupur Srivastava is Chief Operating Officer at Included Health, a healthcare company focusing on delivering integrated virtual care and navigation. After getting her MBA at Stanford University, she became a product manager at Cisco and worked on their healthcare vertical. She felt connected to the mission-driven nature of the healthcare industry and decided to remain in the sector, later transitioning to a leadership role at AliveCor. She has been at Included Health for the past 10 years and remains passionate about raising the standard of healthcare for everyone.

In our conversation, Nupur talks about using the number of days a member considers themselves healthy as a North Star — because “the most important outcome is the one that’s expressed and felt by the member.” She also discusses building “connected hallways” in healthcare so that members can easily flow between products and experiences.
I’ve been with Included Health for about 10 years; I joined as a senior product manager. Over time, I ended up leading the product function, and most recently, I became the chief operating officer leading our tech and operations functions. One of the most important things that I’ve learned is that you have to truly embrace the notion that what got you here won’t get you there. What made someone a really good senior product manager is likely not going to make them a good director and so on.
For example, as a senior product manager you’re probably measured by the impact your product is driving, the way it’s helped the life of the users, and how it’s helped business goals. But the moment you step into leadership, you’re evaluated not on how good of an IC PM you are, but on how effective your team is, how you attract high-quality talent, and how you set the right strategy and drive clear impact on the business through the products you’re building.
Something I’ve tried to be really conscious about as I’ve taken on different leadership positions is thinking about what I need to change to be successful in my new role. The more senior you get, the more you need to focus on clarity and consistency of communication. You need to balance your time between setting vision, anchoring your team to a clear mission, coaching your team, and driving results. You need to focus on aligning your team on a strategy but delegating the execution without meddling in the tactics — you don’t want people to feel micromanaged.
One of my biggest measures of a good leader is how they nurture talent, grow their teams, and bring others into the limelight. You want to causally develop your team to constantly grow and take on more themselves. I spend a fair amount of time doing this in my role today as COO.
I lead the tech and operations functions currently. The biggest thing that I’ve had to learn is where do I add value in each of these functions? How do I support each leader most effectively? And how do I make sure that all teams are aligned against the same strategic goals? A big focus is also making sure that I spend time on a longer time horizon so that we are being strategic and intentional about where we are going and why.
If you think you have to keep doing the same thing, something is wrong. When your role has changed, you have to truly ask yourself and align with your manager on what success looks like in the new role. Then you’ll need to determine what that actually means for behaviors that you need to drive differently.
The first step is ensuring that there’s clarity on what the business strategy is. There’s a difference between business and product metrics and business and product strategy. Business metrics are things like revenue, growth, retention, and margin. In my role on the exec team, I participate in creating the right long-term corporate and business strategy.
We want to make sure we’re not just hitting metrics, but building towards the vision that we have for healthcare. Once the business strategy and the business metrics are set, that’s when product planning kicks in. The product team’s product strategy needs to support the business strategy, and we have to outline a clear product strategy on how they can do that.
In terms of product metrics, we continually work to improve things like user satisfaction, the cost to deliver something, retention, etc. Is the product any good? Are we making our users healthier? Are we driving toward better healthcare outcomes? Are we delivering healthcare at scale? The ownership of these product metrics sits with the product team, so we want to make sure that there’s always a clear line between product planning and business planning.
Similarly, say we’re driving this agenda to move a product metric. We should be able to have a straight-line pathway into which business metric we’re doing this for. What’s the clear reason? It’s a conscious effort to make sure both things are connected because ultimately you want the product team to be supporting both the health and success of the business.
The traditional ways of measuring healthcare outcomes are a good start. A traditional healthcare outcome would be something like, if you have diabetes, are we improving your sugar levels? Or if you’re depressed, are we improving your PHQ-9 (a screening that is done for depression)? We definitely measure a lot of that because that’s how we report our performance back to our clients, but we came up with a metric that is a lot more user-centric: healthy days.
We ask users of our product, “During the past 30 days, for about how many days did poor physical or mental health keep you from doing your usual activities, such as self-care, work, or recreation?” We track how that changes over time as the member interacts with us because ultimately, the outcome that is most important to us is the one that’s expressed and felt by the member. This is our North Star.
We also want to improve outcomes while doing clinical work. Sometimes, a member’s blood pressure is improving, but they may not feel it. And if they don’t feel it, maybe they won’t stick to their meds or improve their regimen. We want to do whatever it takes for members to have literacy in what our clinicians recommend, as well as have them feel a difference in the number of healthy days they can live.
Every healthcare company wants to be the “front door” of healthcare, and I think that’s a ridiculous concept. When someone is not feeling well or is scared or nervous, they’re just going to look for what is trusted, what is easy, and what is known. They want to remove pain and suffering and get back to living.
When we do user research, we see a common frustration around how nothing in healthcare is connected. We’ve all experienced something similar — you might have a primary care provider but end up needing to go to an urgent care, and then later call your insurance company. Every time you go to any of these entities, you have to re-explain who you are. You have to tell them what your issue is again, and there’s no continuity. Everybody will ask you the same questions. This gets even harder if you don’t always remember the details that doctors want to know.
When I say “connected hallways,” I’m referring to the big opportunity we see to break down these barriers in healthcare. When we build our products, we want to make sure that a member can use just one app, whether they want to be seen by a doctor or if they need financial questions answered. We want to build a system that’s connected so that information about the member flows between all these different players. A person’s identity is not that of a patient — they want to get back to living their life, not deal with their financial and clinical parts of healthcare in disconnected ways.
Scale is very interesting in healthcare because I generally think there’s a lot of waste. Simple things like needing to call a doctor’s office to get the source of truth on whether your insurance is accepted or not is really inefficient. There are bloated processes everywhere.
We have a two-tier approach to scaling. One is the classic process and people approach. How are we using process optimization techniques to ensure that everything that we are doing is high value? The second, more interesting, piece is technology. In particular with advances in generative AI, we are seeing lots of opportunities to scale.
For example, today, after our care and clinical teams have a conversation with a member on the phone, we use AI models to auto-transcribe and summarize what happened. We don’t have to spend time writing notes. Not only are we saving a bunch of time and helping scale, but now that the notes are documented, we can use the intelligence in those notes to proactively personalize the member’s future journeys. And we can share a great summary of the conversation with our members!
Healthcare has a lot of components that require a human touch and empathy. We’ll never replace that with AI. We’ll always need clinicians and care coordinators. But we like to believe that a clinician with access to AI will win compared to a clinician without it.
In healthcare, this is a bit easier for us to do because nearly everybody has had a harrowing healthcare experience in their life, even if it wasn’t super serious. There’s a very empathetic group attracted to product roles in healthcare because it’s very mission-oriented.
But, we don’t want to just build products based on our own experiences. We try to do both primary and secondary research to make sure that we’re getting an accurate representation of people’s views throughout the US. We serve clients like Walmart, for example, and the composition of Walmart’s customers is a good representation of the country’s population. And with almost everything in healthcare, when we’ve entered the category, we haven’t looked at competitors. This is because we want to start with the patient’s wants and needs, not what others are doing.
A lot of carriers offer a program called the Care Case and Disease Management Program. This is where if the carrier considers you high-cost or high-risk, somebody will call you to check in on you with the goal of controlling costs. There are many things wrong with this. First of all, few people trust the carrier to manage their healthcare journey because everyone thinks they’re doing it for cost. The entire program is known to have low engagement and low re-engagement rates, and questionable impact.
We wanted to design something better to offer our clients, for our members. We did a lot of research through talking to members going through tough healthcare situations and asking them what they would find most useful. They said that the moment you call something a “disease management program,” you’re identifying them with that disease. But that’s not how they want to be viewed — they’re humans trying to live their lives and they happen to be dealing with a condition.
Even the way you introduce or talk about supporting patients should be different than how it’s typically done. You shouldn’t call them and ask them to enroll in a program — you should instead call them to strike up a conversation, or use the app, chat, and use modern technology to let them know how you can help them.
When we redesigned the program, it was extremely patient-centric. We never asked a patient if they wanted to enroll; we just asked them if we could help them. Sometimes, we led with ways we could help balance their issues and figure out what their insurance covers and doesn’t cover. Within a few months, we were enrolling 3–4X what the carriers ever enrolled and were seeing great satisfaction from our members.
I am optimistic about this. Overall, AI in healthcare is contributing to more accurate diagnostics, personalized treatments, efficient drug development, and improved patient care and management. As technology continues to evolve, its integration into various facets of healthcare is expected to grow, driving further innovation and improvements in health outcomes.
At Included Health, we’re able to move faster on AI because we’ve been using data science in our patient provider match models for many years. We recently went live with a chatbot that can start answering some administrative questions for you. We also have seen the ability to drive efficiencies internally for our care and clinical teams by helping them summarize their conversations with members and we can use these insights to personalize outreach in the future.
There is a ton more opportunity we see and I am optimistic about the future here.
We’ve learned a lot about the growth of telemedicine during COVID, and I think standalone telemedicine is not as interesting as telemedicine integrated within a larger ecosystem. My prediction is that if you are a company that just does telemedicine, you likely don’t have a bright future because it’s another point of fragmentation. The more you can consolidate and integrate, the better.
In the future, I think we’re going to see telemedicine consolidated with other components of the healthcare system — like in-person care or navigation services. There will be multiple services accessible in one place, with telemedicine being one of them. Many clinicians say that a majority of primary care visits can be done virtually, but some patients don’t see it that way. They want to be seen in-person to feel like they’re being taken care of.
I think it’s similar to the banking industry. Previously, we had to physically go to a bank to do anything. Now, we can do most things virtually. But every now and then, if we have a serious problem with the bank or your account, you do want to go in-person or talk to a real human over the phone. I feel like healthcare is moving in that direction toward virtual-first models that will scale access to people who can’t typically get high-quality care.
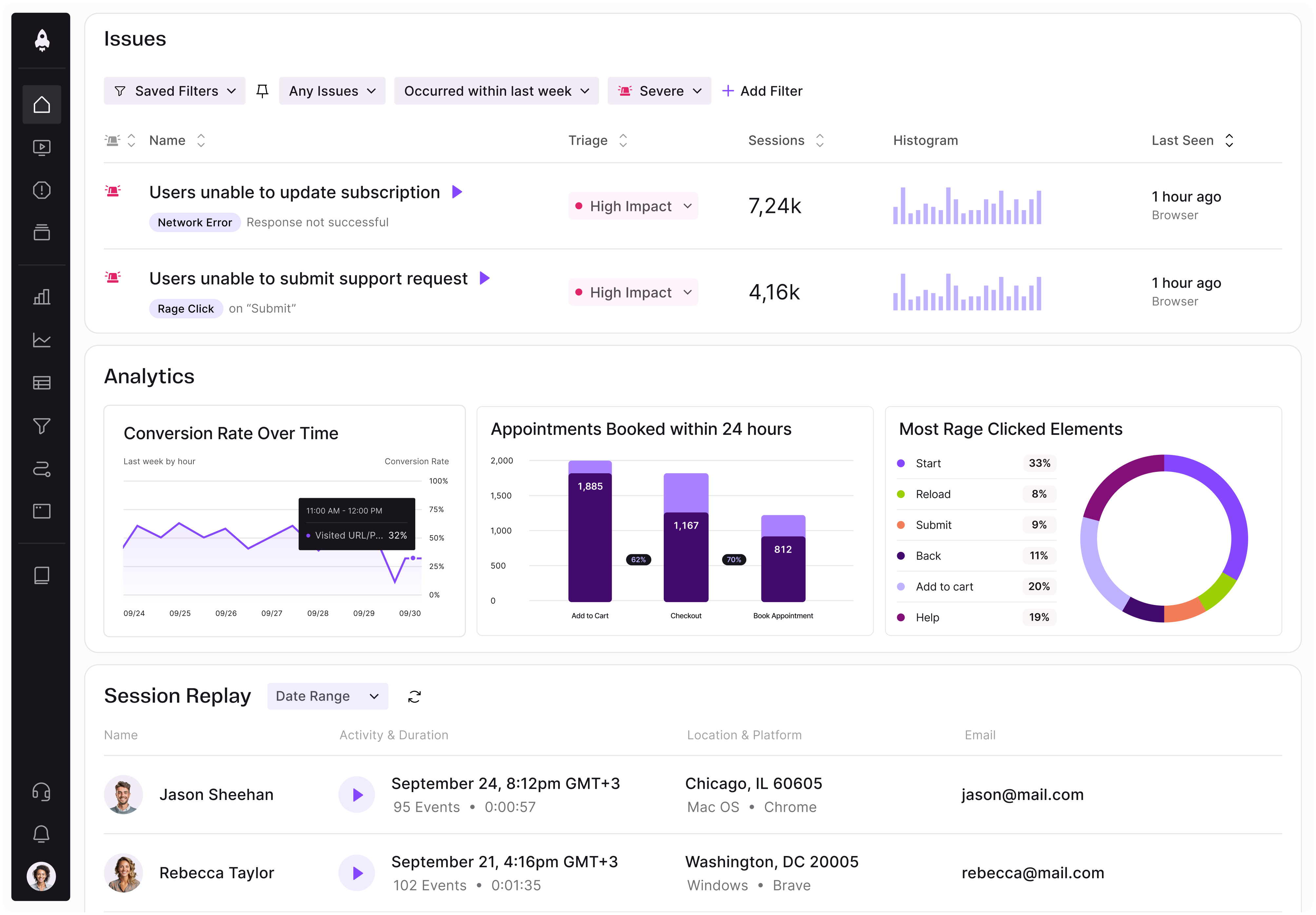
LogRocket identifies friction points in the user experience so you can make informed decisions about product and design changes that must happen to hit your goals.
With LogRocket, you can understand the scope of the issues affecting your product and prioritize the changes that need to be made. LogRocket simplifies workflows by allowing Engineering, Product, UX, and Design teams to work from the same data as you, eliminating any confusion about what needs to be done.
Get your teams on the same page — try LogRocket today.

Rahul Chaudhari covers Amazon’s “customer backwards” approach and how he used it to unlock $500M of value via a homepage redesign.
A practical guide for PMs on using session replay safely. Learn what data to capture, how to mask PII, and balance UX insight with trust.

Maryam Ashoori, VP of Product and Engineering at IBM’s Watsonx platform, talks about the messy reality of enterprise AI deployment.
A product manager’s guide to deciding when automation is enough, when AI adds value, and how to make the tradeoffs intentionally.