Maximilian Maile is Senior Vice President of Digital Health at Parkview Health, a mid-size health system within Northeast Indiana and Northwest Ohio that spans 22 counties and two metropolitan hospitals. He has more than 20 years of experience in leading the digital transformation journey in healthcare and has worked at Parkview for more than a decade. Max began his tenure working on continuous improvement for the system and transitioned to the medical specialties division, followed by virtual health and telemedicine, and more.

In our conversation, Max talks about how Parkview is redefining digital health by providing flexibility for patients to connect with healthcare via technological innovation, interconnected devices, and more. He discusses current challenges facing digital healthcare, including software integration and the spectrum of compatibility between technologies. Max also shares how his team rolls out patient-facing features in a “big bang” fashion to get immediate feedback instead of doing lengthy pilots and trials.
Parkview started its journey with digital health in 2016. At that time, there was a lot of discussion of what digital health meant. Is it telemedicine? Is it virtual health? There was some usage of asynchronous and synchronous visits, but as a whole, it was really around video. We’ve since redefined that as care that’s happening for a patient outside of typical brick-and-mortar healthcare operations. That often looks like care in the home, in your car, on vacation, or wherever you may be.
Since the pandemic, a lot of care now focuses on the home. Back in 2016, we also focused on providing care to community hospitals via a video stream and having a specialist connect to another brick-and-mortar site. That was a case where the care did fall within our brick-and-mortar facilities but wasn’t normal operations. This was a unique way to get a specialist to a different site. Video is still a major component of digital health, but so are devices, connectivity, patient portals, and more that allow a patient to interact with healthcare.
This question is actually debated on a national level as well. Initially, 10 years ago, telemedicine was for rural care. But the reality is that quick access to healthcare can be just as difficult in urban areas with high traffic. So, that mentality has changed. At Parkview, we don’t want to be prescriptive for people one way or another. We just want to provide options for care. At the end of the day, a loyal patient is someone who gets care in the way that they want, not in the way that we necessarily dictate.
Our providers weigh in on what the appropriate visit type is, and there are some instances where you have to be in person. Our goal is to work with our providers and say, “If they’re able to do a telemedicine visit, are you okay with that?” All our providers can do video visits with their patients, although some are more comfortable than others.
I think now, post-COVID, people have been conditioned to be more aware of sickness around them. There are two components to that. First, medically, people are unconsciously aware of people’s conditions around them and if they may be being exposed to something. For example, in waiting rooms in particular, people don’t want to sit next to other sick people. This has always happened, but now people know they’re sitting next to sick people and can act differently in waiting rooms. They may be extra careful to avoid touching objects around them or choose to wait in the car.
Second, we’ve changed as consumers as well. People have different expectations as a consumer than they did when they were just shepherded through the healthcare process. Now, someone may have a high deductible plan, and so spending that money matters more because they’re spending those dollars out-of-pocket. They’re aware of the options that exist and how long they’re waiting when they spend that money. There are also more options out there now — whether that’s for primary care, vitamins, lab testing kits, etc. Many of these are available through simple transactions online versus before when a provider had to see you in-person first.
I have always been entrepreneurial. That component weaves through all the roles that I’ve had over time and my thinking as I’ve approached jobs. I had my own business at one point in life, which was a great experience, and then I moved into a product development role with a publicly traded company. I have three sisters who are all in healthcare and I saw the service heart that healthcare has — the type of people that they work with.
Around 2010, I took a new role in healthcare. It was entry-level, and I worked my way up through our organization through some management roles. Eventually, an opportunity came about for helping to start telemedicine here at Parkview with a couple of other key individuals. That felt very entrepreneurial to me, and I jumped at the chance. The economist in me looked at the healthcare industry and saw so much opportunity for future growth.
It really has been a great fit for me. The team members I work with every day are so important to our success — they’re amazing and I recognize that every day. I don’t personally do the project management or the coding, but our group makes all of that happen. A critical part of anyone’s success is surrounding yourself with people more talented than you and working well together with them. Together, we think in a start-up-minded way where we look at each of our new initiatives like new businesses for Parkview, and that has been hugely successful for us.
Success in healthcare depends on being able to be a collaborative partner with folks and not building things within your silos. It’s an amazing industry — there are so many talented people working both as providers and on the backend. That collaboration is key to making sure that you’re always thinking of who your work is going to impact and getting their ideas and input. Partially, that’s out of necessity — you can’t move something forward without their blessing. But also, to ensure success when you’re changing something, you need everyone’s support. No one likes change to just happen, they want to be part of the change. That’s where the collaboration really underpins your success.
The easy part is going out, choosing a technology, and saying, “We’re going to implement A, B, or C.” That’s one step, but ensuring that people are using that solution and using it to its full capability is a whole other level of success. That’s the crucial part and why collaboration is so necessary.
A difficult challenge right now is not knowing what’s accurate or not when you’re evaluating software and vendors. Integration is a key part of working with our electronic medical records (EMRs). Everyone says they integrate, but what that actually looks like is a huge spectrum. In the case of AI, there’s a lot of, “Is it a locked algorithm? Is it a black box algorithm? Is it machine learning?” That raises all kinds of red flags for us. Those are all different questions. The bottom line is that it’s difficult to know what you’re purchasing and whether it’ll work in the way that you want it to.
The other challenge is not investing too early. Technology changes so rapidly. It’s important to look at the financial impact of things. When you’re looking at the potential ROI and the potential implementation, you have to think about whether we’ll get the reward for that or if there’s something cheaper and better coming along so quickly that we may be overpaying now. There’s a fine line between what’s cool and exciting versus what may not be financially feasible yet.
Pilots are considered a very sound strategy to evaluate the impact that something could have. You start with a small, engaged group and work through the kinks before a larger rollout. That’s an excellent way to get early adopters that are happy to help you work through those challenges that would otherwise be very frustrating to users. You have to iron that out before you roll it out to the masses. I’m thankful that we have providers and groups that are willing to help us test some of that and then move forward.
Especially with EMR changes that don’t impact our staff as much as our patients, we tend to roll those out in a big-bang fashion. If it’s a scheduling change or feature functionality that benefits the patient, we would try to roll that out to the large group. We don’t promote it or market new stuff, we just watch it. Then, with 500-some-thousand users, it gets clicked on pretty quickly. You can see in the background what’s happening and if people are frustrated with it. It’s great to have a large user base with patients in that regard.
It depends. There are always financial implications or an ROI to things, but that may not necessarily be dollars. It could be efficiency or that we make fewer calls to someone because we implemented a messaging feature. Scheduling is a good example of how you reduce the calls to our system by allowing patients to do it online. In the past, we’ve also measured miles saved traveling to a visit, how much time that translates into, and dollars per gallon of gas for that patient. It’s the same for providers. If they have a window of time to drive to a rural site and a one-hour drive back, that is very valuable time for that provider. And if we’re trying to implement something new on our digital devices, we might measure that on patient or provider satisfaction.
Parkview has held an innovation contest for several years around how we can harness ideas from all the bright people who work for us. Receiving the innovation award was an incredible honor — it felt like an acknowledgement of my passion for entrepreneurship and problem solving. Where it really helped, was highlighting that point in my career, where the intersection of patient engagement met innovation. Ever since then, there has been a continual pursuit to continue looking for those opportunities to solve patient challenges with technology. That directly correlates with my role today.
Six or seven years ago, beacons were relatively new. Apple released them so they could sell more iPads, essentially. We had an issue in our hospital, like many hospitals do, where wayfinding was challenging. How do you find your way to a site within a large hospital and find your way back?
I experimented with creating a GPS-like solution using beacons to help direct people through a hospital. The Parkview team later developed this app strategy, incorporating maps and step-by-step directions that come up on the user’s phone. In our health system now, you can hold your phone up and it’ll tell you exactly where to turn and where to go.
The consensus is that digital health is going to continue to grow. There are probably two pieces to that. First, the hope is that it will evolve to be recognized simply as healthcare, transcending the “digital” qualifier. It’s really just a different medium that we’re consuming this on. My goal or hope would be that providers and patients alike embrace it as another way that we can deliver that same high-quality healthcare to people.
The best use of technology is when it creates a better experience for everyone and you don’t even know it’s there. The goal is to allow providers and patients to have a better visit with each other, whatever that looks like, and the technology assists with this in the background.
The second part of that is I hope healthcare embraces it in the same way that the auto industry has embraced technology within cars. Cars now are technology-first vehicles. The future of digital health within healthcare is that we bring those two areas — technology and healthcare — from being different to working seamlessly together — whether that’s handing off from the physical environment to the virtual environment, or whether that’s using them as some sort of hybrid care option.
Other thoughts I have on this are related to generative AI. We’ve used AI for image recognition for years in radiology. We’ve used it more recently in diabetic retinopathy scans that used to be highly inefficient, and now we’ve made them incredibly efficient with a five-minute scan that costs only a couple of dollars. It’s amazing. We’re using AI for voice to help physicians write notes because it’s been proven that the AI can assist in generating a more empathic tone. AI can help craft something that the provider can review before sending it on to the patient.
I don’t think we’ll be having robo-doctors anytime soon, but I think that we will utilize those services in communicating with patients and making those interactions more seamless. That’s my goal and what I think will happen in the future.
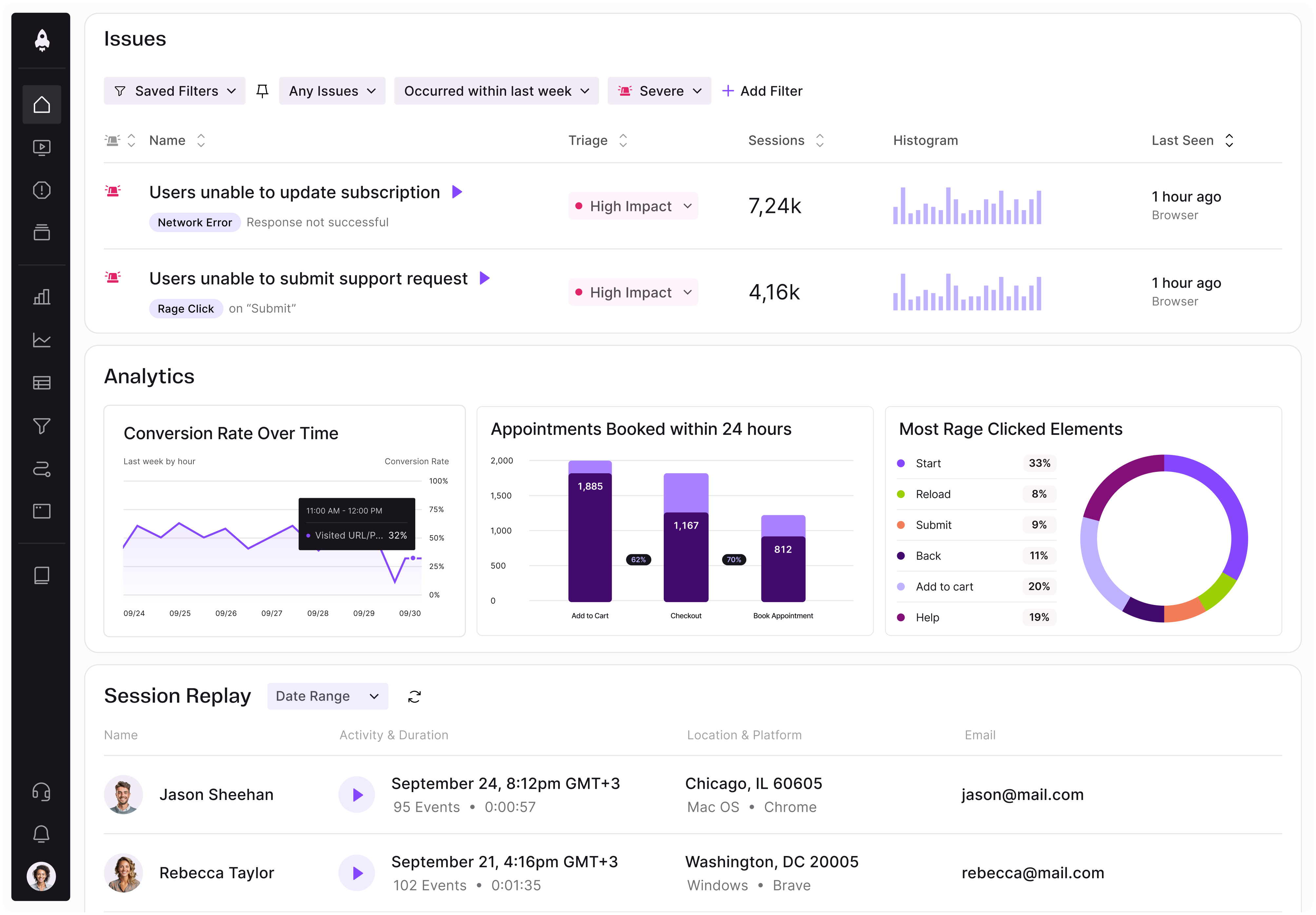
LogRocket identifies friction points in the user experience so you can make informed decisions about product and design changes that must happen to hit your goals.
With LogRocket, you can understand the scope of the issues affecting your product and prioritize the changes that need to be made. LogRocket simplifies workflows by allowing Engineering, Product, UX, and Design teams to work from the same data as you, eliminating any confusion about what needs to be done.
Get your teams on the same page — try LogRocket today.
A practical guide for PMs on using session replay safely. Learn what data to capture, how to mask PII, and balance UX insight with trust.

Maryam Ashoori, VP of Product and Engineering at IBM’s Watsonx platform, talks about the messy reality of enterprise AI deployment.
A product manager’s guide to deciding when automation is enough, when AI adds value, and how to make the tradeoffs intentionally.

How AI reshaped product management in 2025 and what PMs must rethink in 2026 to stay effective in a rapidly changing product landscape.