Dr. Deepti Mehtani is VP, Clinical & AI Solutions at NextGen Healthcare, a provider of innovative healthcare technology and data solutions. With a background in medicine, Deepti earned a Master’s in Hospital Administration before transitioning into product management for healthcare companies. She worked as a healthcare consultant at Infosys Public Services before joining Amazing Charts as a business analyst. From there, Deepti held various product positions at companies such as CareCloud, Medidata Solutions, SHYFT Analytics, and Kipu Health before assuming her current role at NextGen Healthcare.
In our conversation, Deepti talks about how her background as a clinician helps shape product strategy at NextGen Healthcare, including how she uses her own first-hand experience to address challenges like alert fatigue and technology barriers. She also discusses her priority to design products that give clinicians time back to focus on their core work: patient care.
Integrating the voice of the clinician into the process is crucial for creating solutions that are genuinely adopted by healthcare professionals. We want our technology to help their workflows rather than act as barriers. To do that, we use frameworks such as clinical persona and empathy mapping. Human-centered design, agile methodologies, and continuous feedback loops are also big elements in our work as well.
Persona and empathy mapping specifically help us put ourselves in the shoes of the user — understanding what they go through every day and what their most important tasks are. We also learn the challenges they face and the redundant elements of their work. We want to ensure that the product serves the users well, rather than the other way around where the users are working for the product. We have seen that more often than not.
We also embed their feedback and our goal is to make features that are relevant to the diverse needs of clinicians. We have so many specialties, including orthopedics, pediatrics, primary care, dermatology, and more. In some places, physical exams are more important and in others, lab tests are more important, so that context is important depending on the specialty.
In terms of human-centered design, we think about challenges like alert fatigue. How do we ensure that the right information is presented to them at the right step in their workflows? With continuous feedback, we validate our designs with the providers. We do focus groups, interviews, validations, and more. Ultimately, we want to ensure that we incorporate user feedback into our product strategy and build to the specifications.
When talking to providers and asking them about their biggest challenges, the vast majority of them say technology! Instead of helping them, technology is actually a barrier. They’ve shared that EHRs are creating more challenges for them than they’re solving. So, we first focus on breaking this down. What do they mean by disruptive, challenging technology?
At heart, clinicians are focused on giving care to the patient. That’s their main priority. They want to be able to talk to patients and focus on their care, not be burdened with documentation, especially in our world with payers, reimbursement models, etc. From their understanding, these are complex user interfaces — there’s poor usability, documentation is time-consuming, and it leads to burnout and cognitive load. So, how do we address that?
First and foremost, we work in partnership with clinicians. We want to understand their biggest challenges and surface information at the right steps in each workflow for them. Instead of showing everything at every step, we want to make sure it’s all context-based. Further, we want to reduce the number of clicks. In some cases, this is tricky because that means we’d have to display more information, so we approach this with a balance. If reduced clicks would increase cognitive load, we might go with a cleaner interface instead. It’s all about context.
Yes, definitely. We were recently working on a feature where my team ran some designs by me. They were beautiful, but one of them was forcing the user into a specific workflow. I said, “What if the clinician doesn’t want to go through the workflow? Where is an alternative or an out for that?” They said, “But most of our providers use this workflow, so it’s OK.” I was persistent and said, “But if I wanted to exit out, you are not giving me a way to do that. I’m being forced to go through it, which adds five extra steps.”
They said, “Actually, we didn’t think like that.” As a clinician, I may be going through that flow 70 or 80 percent of the time, but sometimes, I can ask someone else to do it for me. So how do I exit out and save myself these extra steps? It was a good opportunity for the team to see how I was thinking, and then they went back and revised the feature before it went into development. These things really help. My background and mindset help us see things that we might not otherwise.
With everything, I focus on three key factors. The first is looking at the real-world use cases. Instead of solving a phantom problem, I want to look at what clinicians are doing and how we help them in their existing workflows. We want to avoid saying, “Oh, here is a cool thing we built for you. Do you want to use it?” Focusing on real-world use cases is very important to ensure we help them do their job before giving them extra features.
Second is a feasibility check. Is it going to save time? Is it going to help improve patient care? Is it going to increase administrative burden or actually help them? Third, how is it going to work with their existing systems and impact IT resources? Their existing technology integrates with labs and tests, so if our product is disruptive to those things, they’ll have to go outside of it, which isn’t practical or beneficial.
I recently acquired our mobile team as part of the clinical team, so I’ve been learning how our mobile app works, where our training material lives, etc. As soon as I logged in, I said, “OK, where are the tutorials?” When we got to the page, I quickly gave feedback to my team and said, “It’s amazing that we have all the tutorials right here at my fingertips. I can see the title of the tutorial, but it would help if I could see how long each one will take me. That way, I’ll know how much time I am going to invest in this. If it’s a minute long, I can see it in between patients, but if it’s 10 minutes long, I’ll need to watch it during my lunch break.”
As soon as I come into a product, my first thought is always “how much time do I need to invest in the tool or feature?” As a clinician, I think about how I’m going to manage my time. How many tasks can I complete in between patients or during lunch so I don’t have to do it at home?”
This is an important question because the right team helps you build an effective solution. One of the qualities that I look for is a clinical healthcare background. They need to know what happens on the scene. I like to see that they’ve either worked in the industry before or have experienced it in one way or the other. That way, they appreciate the challenges more and understand pain points better, motivating them to solve these problems.
Next, I look at what drives them. Do they have a passion and mindset for solving problems or do they just view this as a job they have to do? And what kind of product management skills do they have? Healthcare is a complex ecosystem with challenging requirements. There are patients, providers, and payers in our equation. We need people who can understand the challenges and workflows for each persona and translate that for our technical folks who will then build the right solution.
EHR has a lot of features, and just as I mentioned that we offer tools for different specialties, we are also going to introduce different age groups into our product design. Let’s say for example, we’re talking about proactive, preemptive screenings. Those all happen at different ages in one’s life. For example, pediatrics is more focused on vaccinations for newborns at certain months, and other vaccines come years later, etc.
As we move further along our lives, we all go for more preventive measures such as mammograms and colonoscopies. These are patient care and preventive screenings, but they can also become care gaps if they’re not done at the right time. Care gap identification is important to see if someone is missing a procedure or screening. Lots of systems have these features and modules, but they may not be presented to providers at point of care.
For example, if I’m holding a visit with a patient and a care gap is flagged while I’m preparing to see them or while interacting with them, I would be more inclined to prescribe those medications or schedule those screenings at the moment. Otherwise, if I see the care gap after the patient leaves, it’s harder to go back and get that all scheduled.
Medical histories create a different gap because providers will have to manually read and prepare for visits upfront. Now, our system can provide those datapoints to them while they are with the patient in the room at the point of care. After talking to a lot of providers and even experiencing this myself, we realized this could improve.
This is part of what I mean when we say that our product is trying to be context-based — prioritizing what needs to be shown at the point of care to the provider so they don’t create any care gaps. We want to address this issue and prevent poor patient outcomes from these gaps or oversights. So, we designed a solution that would present directly in their workflow and create personalized care plans based on a patient’s attributes, age, family history, and health history.
Have they undergone any surgeries? Do they have chronic pain or conditions? We also took the payer’s insurance guidelines into account, as well as clinical guidelines, to create personalized care plans for these patients.
In this process, we have to prioritize these points but make sure they’re not obtrusive to the workflow. Providers need to see them but not have to take action on them before moving on to the next step. So, we had to be very careful in our design and validate all of these decisions with our providers. On top of that, we had to make sure we’re complying with regulations at the same time.
AI and ML, for sure. You might have noticed that AI is already making an immense, profound impact on healthcare. We can’t even measure that potential right now. We have seen how it is helping already in documentation workflows, for example. There are enhanced voice recognition tools, ambient technology, and seamlessly converting verbal inputs. When I go visit some of our customers, they don’t even need to touch the technology — they can focus and have it running alongside them without them needing to interact with it.
At the end of the visit, they stop the recording of the scribe tool, review it, and sign off on it. That documentation helps them in feeling like they are providing the right patient care and assuming less burden. This has also changed the patient experience as well. AI and ML are enabling patients to have better patient portals where they can schedule, reschedule, search for appointments, access health records, look at their medications, and more. Yes, this helps clinicians too, but it’s great for patients. And that’s the central point of what we do — we are serving the patient at the end of the day.
Our AI-based NextGen Ambient Assist is used by 1,500 providers every month. We have 1.5 million patient encounters annually as of now. Our tool supports different languages and creates structured notes based on the provider’s preferences like paragraph style, tone, and more. It also suggests diagnostic codes and orders management.
Overall, we’re seeing immense impact on the way providers use these systems and how they can leverage Ambient and other AI technologies to be more efficient. Providers have told us that it saves them over two hours a day in documentation. They are going from visit to visit and are finishing their documentation simultaneously.
This is just the beginning. We have much more coming out this year. There’s tremendous potential for using these technologies and enhancements in our day-to-day lives.
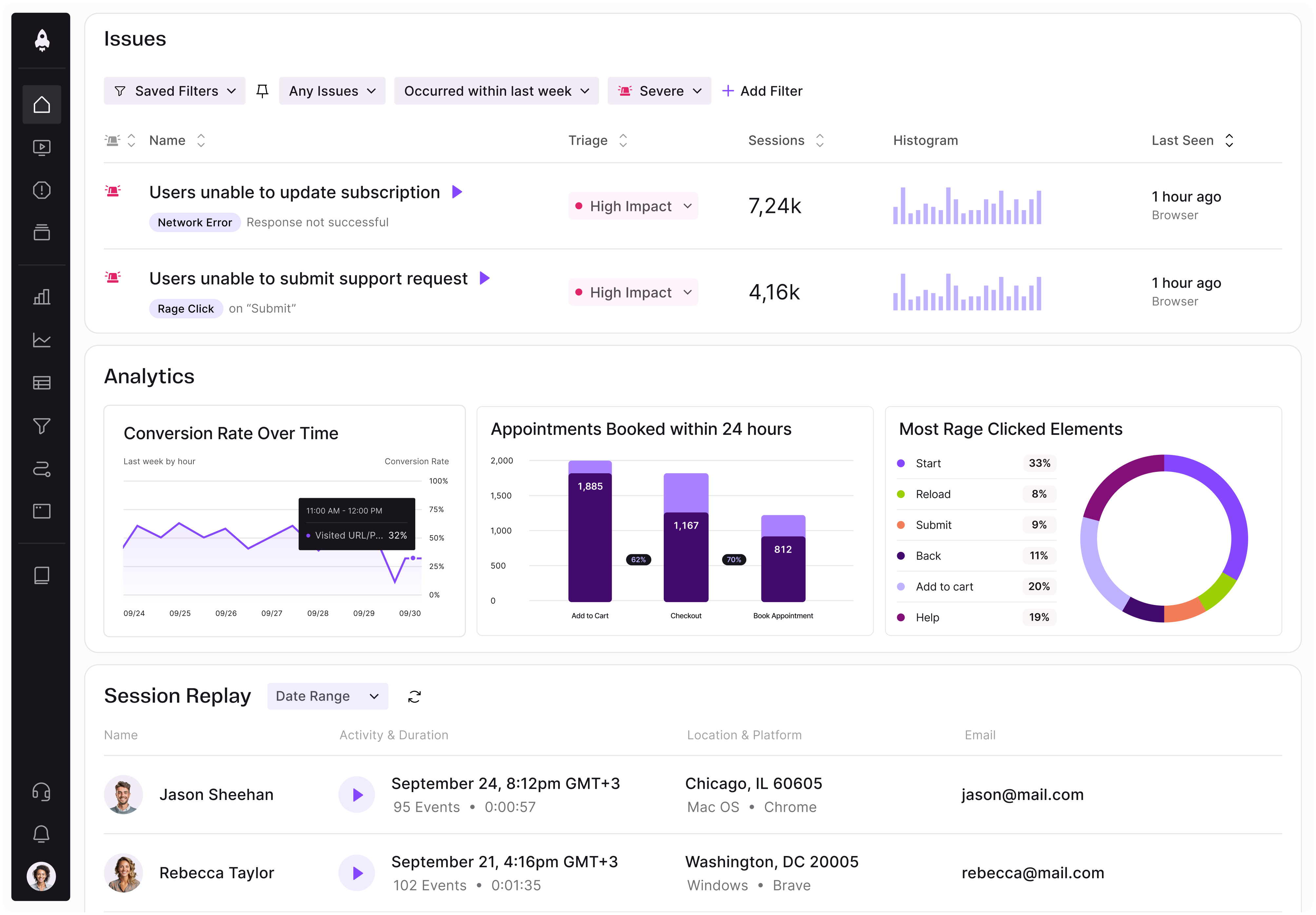
LogRocket identifies friction points in the user experience so you can make informed decisions about product and design changes that must happen to hit your goals.
With LogRocket, you can understand the scope of the issues affecting your product and prioritize the changes that need to be made. LogRocket simplifies workflows by allowing Engineering, Product, UX, and Design teams to work from the same data as you, eliminating any confusion about what needs to be done.
Get your teams on the same page — try LogRocket today.

Rahul Chaudhari covers Amazon’s “customer backwards” approach and how he used it to unlock $500M of value via a homepage redesign.
A practical guide for PMs on using session replay safely. Learn what data to capture, how to mask PII, and balance UX insight with trust.

Maryam Ashoori, VP of Product and Engineering at IBM’s Watsonx platform, talks about the messy reality of enterprise AI deployment.
A product manager’s guide to deciding when automation is enough, when AI adds value, and how to make the tradeoffs intentionally.