Daric Snyder is the Director of Experience Design in the digital division of Emplify Health, a not-for-profit, patient-centered regional healthcare system. He began his career in digital media, working for the National Press Foundation and as a freelance designer. Daric then became the online director for Baltimore Magazine before launching his own news product, Baltimore Rex. Before his current role at Emplify Health, he was the Director of Customer Experience at CPower Energy.
In our conversation, Daric talks about how his team is developing supportive, user-friendly healthcare software that layers on top of traditional health records systems, which can often be difficult to navigate. He also highlights the complexity of designing solutions that meet the needs of both providers and patients, especially across such wide and varying demographics.
A few different things have come together in the last few years at Emplify Health, with COVID being one of them. As an organization, the pandemic pushed us toward digital adoption and forced us to look at how we engage with patients online.
The other aspect was the merger of equals we’ve undergone that brought two successful, regional health systems, Gundersen Health System and Bellin Health, to become one system. While the right direction for future system success, this merger came about during a very turbulent time for healthcare.
We wanted to hold onto the best of what we were doing at the moment while still working toward the future. Emplify Health serves 11 hospitals and 100 clinics across Wisconsin, Minnesota, Michigan, and Iowa. We have about $3 billion in annual revenue, 15,000 employees, and 100-plus years of history. We’re not a tech company or even a tech product-focused organization by nature, but our executives had the great idea to adopt product approaches and methodologies into our practice.
We focused on bringing UX into our existing healthcare expertise, as well as building agile product and solutions teams. The first iteration of this change was around changing our virtual care offerings, revamping our website, and bringing human-centered design skills to the table.
To do that, we had to think about what we were really trying to solve in this space. Some of our projects were more consumer-facing, but we also tried building initiatives to go after internal teams. We had a team focused on improving the experience of the frontline hospital staff coming out of the pandemic. Last year, we kicked off an approach with our pharmacy service line and set up a team there. We’ve learned that we can’t just take an existing team, send them to an agile boot camp, and have them flip the way they work. We brought on a lot of additional support, which helped everyone adjust to our new way of working.
A big part of success in this area is building teams with autonomy and freedom of motion. If you’re coming from a command and control or waterfall approach, it’s hard to make that shift to complete autonomy. We want to let our teams and team members prioritize their work; our goal is to get out of their way while still supporting them.
It’s also important to recognize that if that team has a lot of dependencies on their day-to-day operations, whether it’s another team or the organization altogether, they won’t have autonomy. You’ll just end up in the same structure as before and continue dealing with the same problems. For this to work, you need to find out who you need on the team and who else has to be aware of what’s going on.
It’s really hard to get to a place where you’re truly responsive and customer-centric. This is a great place for a product analytics tool, like what you all do at LogRocket, to measure and observe customer behavior. The data points you get from tools like this help you track usage and what’s actually happening within your product. Especially when considering financial metrics, tying these behaviors to those outcomes is critical.
Along the same lines, introducing qualitative data and insights is also important. You need qualitative data to have a deep, shared understanding of someone’s product experience. In healthcare, particularly, there’s still a lot of dependence on surveys. These can help, but you don’t get the same types of insights as if you were sitting down and talking to people.
As a result, we’ve implemented a lot of methods to go out and talk to patients directly. We want to show them what we’re working on and discuss topics we think would be good for us to know about. One of the big challenges that we’ve spent a lot of time on is breaking down barriers and building trust with our patients so we can create strong, rapid feedback loops.
There was a huge explosion in realizing that the old, pre-COVID model isn’t going to work anymore. Organizations like ours had to pick up a lot of solutions from vendors to fill in our gaps, such as virtual care offerings or chatbot solutions. We found where we needed things immediately, and in some cases, very early on in the pandemic, heard stories about how teams came together to deliver a solution in just days or weeks.
With that said, lots of companies learned that just adding a bunch of capabilities to what you were already doing and sprinkling digital components over the top doesn’t mean you’ve transformed. It doesn’t mean you’re going to get people to use your solution. Online scheduling of in-person appointments has been a strong example of that. You can’t just flip that switch — you have to work on the underlying challenges around access. How are schedules set up, and how can you show which providers are available? If a user’s first experience is bad, it’s really hard to convince them to come back and try again.
Well, there could be a couple of different reasons for that, and a challenge for us is often to recognize that our patient base does not speak with one voice. They want a lot of different things because our user population is made up of a wide range of people. There are many different demographics and comfort levels with digital offerings. There might still be things that work for subsets of the population that you’re trying to address, and these things might meet their needs very well. Even if it’s a small percentage, if you help get them where they need to go and alleviate pressure on other channels, it’s successful.
At the same time, there are other scenarios when something you put out into the market does not resonate with users at all. That’s when you have to ask, “If we’re not getting an ROI on this, why are we doing it?” There’s been a lot of pressure within healthcare to offer something because everybody else offers it, without actually going in and making sure that it meets the specific needs of that organization’s population.
I’ve worked in quite a few highly regulated spaces, including an energy management company. At Emplify Health and other healthcare companies, navigating all of the impacts of HIPAA and the 21st Century Cures Act is tricky.
A couple of years ago, we were working through how to do web analytics while still keeping patient privacy and security in mind. There are so many added layers of security in these spaces that don’t exist in a direct-to-consumer site, for example. That took a lot of partnership with our vendors, legal team, security, compliance, and more. We got into the weeds to understand the mechanics of everything.
Another thing I’ve spent a lot of time balancing is the needs of care teams and patients. We have to consider both groups at the same time, constantly. At the center of that is an electronic health record system, which is the core of our infrastructure. Frankly, these systems are not built from a user perspective. Everything we want to do — to support our clinicians to do their jobs well and to support our patients in effectively using the patient portal — is built on top of this health records database. We’ve made a lot of progress in a short period, but when the core of this system is not built for these purposes, we’re constantly battling against it.
We use a metric called pajama time, which is how much time doctors have to spend after hours in their pajamas working on that day’s documentation. Sometimes, they’re lucky if it’s from that day because they often have a backlog. Anything new that we offer to patients contributes to this problem, and we have to be very mindful of how our changes affect our care teams.
Yes. The one that’s been the most visible beyond our own walls has been the primary care model disruptors. These are spaces like CVS, Walmart, and Amazon’s One Medical that offer a form of primary care and virtual care. They’ve all pulled back from that over the last 18 months because it wasn’t addressing people’s real-world needs and their existing behaviors.
That’s something we’ve continued to think through — the primary care relationship and where it fits into the ecosystem. As far as new entrants coming in and disrupting the space are concerned, we haven’t seen that yet. However, I’ve found that the asynchronous care model has been undervalued and underpiped. This goes back to pajama time — that burden on clinicians around patient-to-care team messaging. This has been available before the pandemic, but that behavior skyrocketed during COVID and hasn’t stopped.
On one hand, it’s very satisfying to patients and has benefits for care teams too. However, it’s also a new, relentless stream of work sitting outside of what has historically been the way that our insurance-based model pays for care. Figuring out how to navigate that in a way that feels like a win for everybody has been really challenging.
There are two different areas to this. One is, as you hit on, the concern around the digital divide; there’s a substantial lack of broadband internet in some parts of the US. There’s unreliable cell phone service and no broadband in a lot of the countryside, and we have patients from these areas who have long commutes to their nearest clinics. If you’re committed, like our organization is, to providing that population care, you have to figure out touch points or other kinds of interventions that may help create access to care.
Our organization recently partnered with community groups that provided tablets to seniors with built-in cellular modems. It’s interesting to see where those pilots will go. We haven’t seen any definitive results yet, but it’s a great initiative. Likewise, my team has been working to understand the healthcare experiences of our limited English-speaking patients, which includes Hispanic, Somali, and Hmong communities. It’s been really illuminating to partner with our interpreters, translation services teams, population health groups, and others to engage with these patients in their communities.
For example, one of the things we’re learning is that simply translating our website or patient portal content doesn’t always make sense. If these populations are also not digital natives, we’re not fixing the problem. If we’re trying to ensure that preventive care needs are met and that people are not no-showing for their appointments, other methods are going to be more effective.
Yes, there are absolutely patterns and personas to be conscious of. Of course, we also need to make sure that we’re not creating an imaginary person or need. The anecdotes are really useful, even when they’re coming from a fairly specific subset of a population.
For example, we’ve been doing some work on chatbots and virtual agents recently. We had a patient tell us they would rather have a lobotomy than use a chatbot to schedule an appointment. Does that mean that we don’t need a chatbot available to schedule appointments? No, of course not. We recognize that this won’t be the experience for everyone, because we know that younger people would much rather schedule online than pick up the phone to make an appointment.
We know that we have to adjust to different population needs and think broadly about what’s necessary. I find it helpful to draw things back to our overall strategy and recognize that we’re solving different problems for different needs. The needs of our working parents who have young children, for example, are going to be different from seniors who may have a lot more contact with the healthcare system. With that said, they also expect to talk to a human when they reach us, whether via phone call or a chat on our patient portal.
You have to be absolutely clear on your high-level goals and outcomes, and then work your way down. It’s easy to pick a number and say you want to make it go up, but if it doesn’t tie back to the outcomes that you want for the organization or users, it’s pointless.
One of the nice things about working for a nonprofit healthcare system and not for a social media network, for example, is that we’re not just driving engagement for the sake of engagement. If something empowers our patients to make better decisions and get better care, we have to find the right metrics that align with that. From there, we can tell that story all the way up to improving patient access. We can say that we have a theory on how to improve overall community health scores, and everyone working on it understands why we’re doing it. It’s a very empowering job, and I’m grateful for the teams I work with.
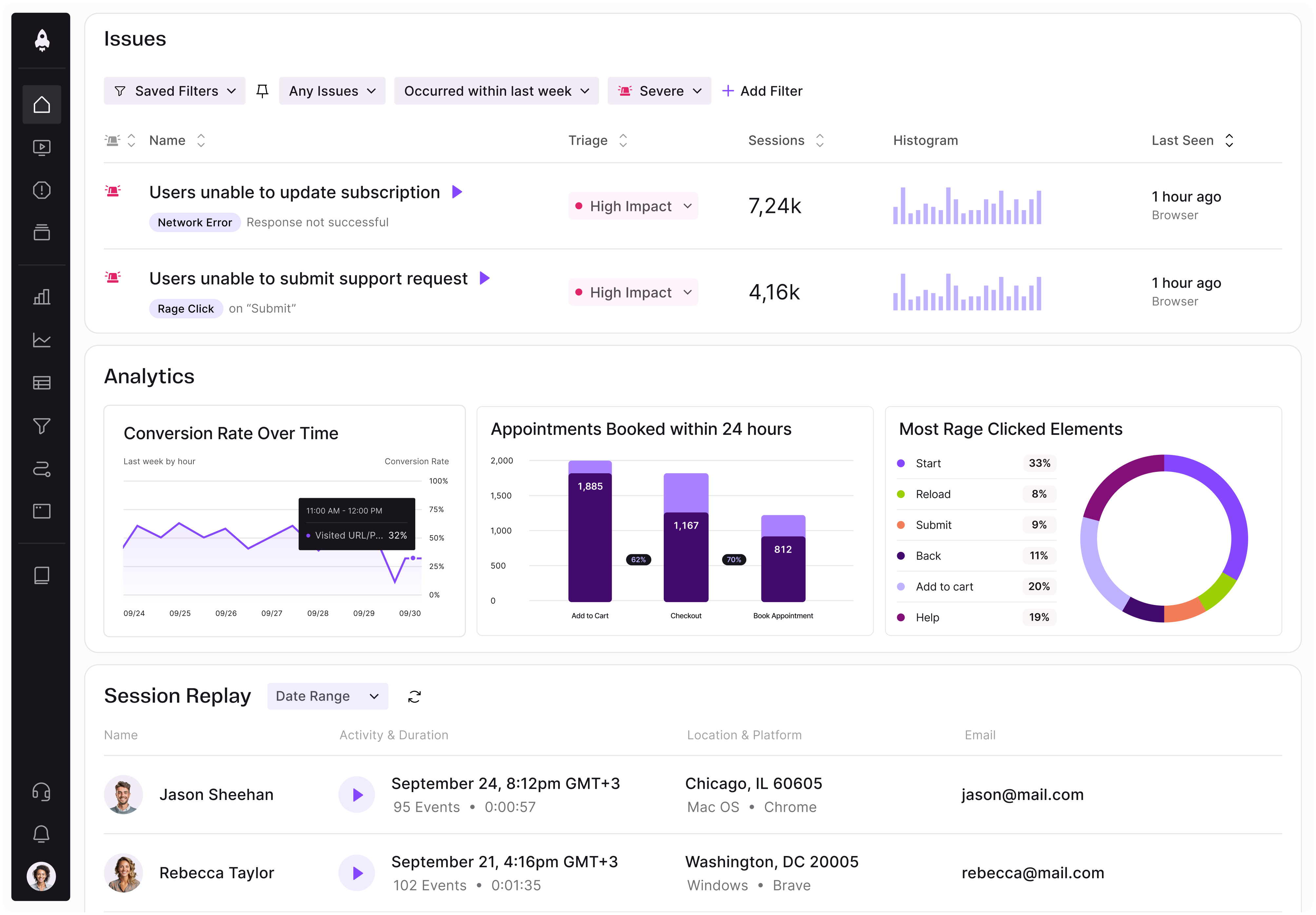
LogRocket identifies friction points in the user experience so you can make informed decisions about product and design changes that must happen to hit your goals.
With LogRocket, you can understand the scope of the issues affecting your product and prioritize the changes that need to be made. LogRocket simplifies workflows by allowing Engineering, Product, UX, and Design teams to work from the same data as you, eliminating any confusion about what needs to be done.
Get your teams on the same page — try LogRocket today.

Rahul Chaudhari covers Amazon’s “customer backwards” approach and how he used it to unlock $500M of value via a homepage redesign.
A practical guide for PMs on using session replay safely. Learn what data to capture, how to mask PII, and balance UX insight with trust.

Maryam Ashoori, VP of Product and Engineering at IBM’s Watsonx platform, talks about the messy reality of enterprise AI deployment.
A product manager’s guide to deciding when automation is enough, when AI adds value, and how to make the tradeoffs intentionally.