Christina Valls is Product Strategy and Operational Enablement Director at Cedars-Sinai, where she is one of the founding leaders of the Consumer Digital Innovation function. With experience at Epic, Cedars-Sinai, and health systems across the US, she has led transformations that expanded access, modernized digital platforms, and integrated product-driven approaches into complex healthcare organizations.

She began her career at Epic, where she worked as a project manager on healthcare technology solutions, product development, and clinical workflows. Christina then led process improvement efforts for UW Health SwedishAmerican where she was responsible for developing and launching a new lean management system for the organization. She has now been with the Cedars-Sinai for nine years, serving as a manager of digital and strategic products and programs before stepping into her current position.
In our conversation, Christina shares how her teams have transformed digital experiences at Cedars-Sinai, including building a digital scheduling platform, optimizing the Find a Doctor experience, and redesigning a mobile app. She also talks about the importance of tying data to both patient outcomes and business impact.
Historically, in healthcare organizations, the approach to implementing and creating new technology has been project-based. As a result, it ends up being a large initiative. You have to plan everything in advance and foresee problems before you implement them.
At an innovative place like Cedars-Sinai that’s running a lot of pilot programs, you’re also working with new companies and trying to stay at the forefront of technology. However, if you don’t have a process in place to ensure that you’re looking at scaling and adoption, sometimes, you end up with many pilots that don’t have the necessary analysis structure afterwards. So, how do you analyze them? Should they be turned down? Should they be scaled? What’s the impact? How do you move forward?
Part of creating a product function in healthcare allows you to take a different approach at solving problems. You’re focusing on the true problem that you’re trying to solve. How do you find the right data to understand and inform the actions that you should take? Then, you evaluate the impact of those actions after the fact, so that you can continually learn and iterate. A big aspect is analytics and ensuring that you’re tracking things, understanding how people move through the journey, where they’re struggling, and where they’re able to get through quickly.
A product function in healthcare brings this all together. It allows you to have a different lens — it’s not just about turning on a technology, but figuring out how to solve a problem using it. You can then create an ongoing relationship and infrastructure to support that approach to innovation.
At Epic, I was shoulder to shoulder with surgeons, anesthesiologists, PACU nurses, and the whole perioperative staff. I was walking the hospital floors, working with researchers, and really understanding the ins and outs of a healthcare system from deep experience. I saw what people are doing, where they struggle with technology, how they interact with patients, and what stressors they encounter providing healthcare for people.
That has really informed how I approach the technology that I look at. For me, it’s never about a technology; it’s about how that technology enhances the relationship between the clinician and the patient. It all comes down to the care that the patient is receiving and how technology helps enable that. That informs a lot of my experiences in product.
I find that sometimes people can get overly ambitious when it comes to healthcare products and what they want to do. You really have to stop and say, “How does this integrate into a clinician’s workflow? How does it help support that relationship? Does it help bridge the gap between what a patient is doing and what the provider is asking them to do?” How do you look at the technology to help break down barriers and provide the necessary support? Technology shouldn’t be the end-all-be-all — it’s about the care that’s delivered and how technology supports it.
With that said, startups and folks who have experience in the industry want to move fast. While that’s an excellent approach, we always have to remember that that trust in that relationship is the core to what we do.
We started by aligning on key outcome metrics. Since we’re building a framework for the team to tap into from scratch, we had to tie in organizational, department, and product-level goals together to create clarity around what success looks like, especially as we can ladder up across all of our different teams to broader impact.
We focused on not only defining what those goals are and creating that ladder, but how to build the habits with the team, like defining hypotheses, tying those to measurable success, iterating with intention, and more. We’re also building up our data capabilities so we can track results and adjust in parallel with delivery. We start small, grow that impact, and test, learn, and iterate from there.
In healthcare, you have to earn the right to iterate. It’s a different way of working and approaching problems. We’re always asking, “What’s the lowest risk iteration we can launch?” It still has to protect trust. We don’t have the opportunity to fail fast in healthcare because a lot of these experiences might be tied to a user’s first interaction with the health system. If those experiences are confusing or unreliable, it can make it harder for patients to trust the care that follows. We have to respect that and make sure that our bar is set a little bit higher.
I’m really excited about the introduction of this function in our org. It allows us to take a different lens to look at it from a tech enablement perspective. How are we enabling the business and those relationships? How are we enabling the patient experience? We can focus on bringing together the needs of the business, operations, technology, etc, and find the right approach to intersect all of it.
Within our group, we have three focus areas:
To support these goals, we have a great team of tech development, web strategy, business strategy, product, business operations, technical project managers, design, and more, and we bring it all together with an agile based approach to delivering technology.
We built up a strong UX and analytics function. We’re trying to look at it and decode those qualitative and quantitative signals to tell the full story of what’s going on for the patient so we can help remove that friction.
In being able to understand the data, how people are interacting with the tools, where they’re dropping off, where they’re struggling to move forward, and where there are slowdowns between steps, we can take that data back and have informed conversations with our executives and stakeholders. When we talk to them, we have contextual data to come behind us, and that has really shifted the conversation a lot.
Empathy for the patient, strong healthcare business acumen, and the ability to navigate complex constraints are the most important factors. We need people who can creatively problem-solve at the intersection of tech limitations, clinical workflows, regulatory requirements, and user needs. The magic happens when someone can connect all of those dots and still move work forward.
It always comes back to the whole ecosystem and where to make changes within it. How do we make sure that we’re prioritizing areas that move the needle? We make a fundamental improvement for the patient, but in doing so, we can’t neglect the clinician experience either. If we build a technology that’s wonderfully designed and is gorgeous from the patient’s perspective, but the doctor doesn’t use it or bring it into their conversation with the patient, we haven’t enabled a powerful connection through technology. That’s what our role is all about — making sure it all comes together.
When I was asked to take on driving the growth of online scheduling, I realized we needed a different approach. We’d been trying to do this for six or seven years, and adoption had really stalled. We weren’t seeing any meaningful gains in patients or doctors doing online scheduling. We had more of a piecemeal strategy with little operational buy-in.
I took a step back to evaluate where things were going in the market. We knew we were behind in terms of offering scheduling for healthcare, so we needed to make sure that we were not treating this as a onetime tech rollout. So, we sought to reimagine what we were doing as an access redesign paired with a product thinking approach, to bring together every stakeholder that was involved in this to bring it to fruition.
We started by analyzing the consumer expectations around scheduling. We looked at how people schedule things in other aspects of their lives, like through OpenTable. They bring those same expectations to healthcare tech, so we had to understand those gaps, wants, and needs, as well as our own operational behaviors.
Scheduling healthcare is a really big deal. You have to have the right insurance authorizations. If a patient cancels an appointment last minute, the system ends up with a lot of white space on the schedule, and especially when patients see a shortage of appointment availability, you have to make sure that if a patient isn’t able to come in for an appointment, some other patient who needs one is able to get in. There was a lot of fear that people wouldn’t be able to schedule correctly, and a lot of that has to do with the complex prerequisites needed before you can even get in the door for an appointment.
To help alleviate some of that fear, we launched a new appointment review process with clear SLAs for patient callbacks if errors occurred. We knew that we weren’t going to solve all of that out of the gate, but it could provide a cushion between the point of scheduling and the appointment for a human to review it. We could get that flywheel going with an appointment review process to catch any inevitable errors.
From there, we wanted to translate that to the consumer side by simplifying flows and reducing friction. We looked at our UI so we could make it more intuitive and mobile friendly. With that, the biggest shift wasn’t technical; it was cultural. We turned this into an ongoing program. It wasn’t just about building a platform for online scheduling; it was a program for how we think about how consumerism, scheduling, access, phone calls, and online scheduling all come together. We also evaluated incentives or value-adds.
We implemented an automated wait list, so if someone canceled, that spot fills with another patient. We had decision trees for the schedulers on the phone so that they can get out of paper binders. We launched those all together so people could get a whole package of scheduling tools to help amplify the process. That wrapped everything together in a holistic way that also considered how behaviors are changing and what people expect from their healthcare.
This is another example where we approached a project as a holistic experience. We had an initial focus on redesigning the UX based on user research and journey analytics. The goal was to streamline navigation and improve clarity. We wanted to put key features in places where patients are looking for them contextually, to improve our provider bios, and optimize both the provider and location search experience.
Overall, we focused on the key pieces of information that patients are looking for at different moments in time. If they’re looking for a provider, what helps them make the decision? How do we surface reviews or areas of expertise to help them find the right fit? How do we include more doctor photos so patients can see their faces and get a sense of who they are?
We knew from the beginning that data would be at the heart of this experience. After an initial phase focused on analytics, UX, and front-end improvements, we turned our attention to the deeper structural elements, specifically, optimizing our provider data ontology. While we had already built in tracking and addressed average use cases, we were now seeing that patients often search at the extremes — either very generally or for highly specific conditions that Cedars is known for.
With that in mind, we’re now focusing on making it easier to guide patients when they’re looking for doctors who have specific expertise areas. How can we transform that into a guided search experience? It’s been important to look cross-functionally. We’re starting to take a different approach to that ontology and are working with marketing, clinical, and business partners to make sure that the data is right for the patient’s needs and the system’s goals.
The product manager who led this initiative did an outstanding job unpacking the mobile app strategy. He introduced a dual-track approach that was very well received, which looked at short-term usability enhancements and building toward a long-term modular platform that could support advanced personalization, analytics, and integrated capabilities.
Our vision was a world where managing healthcare is effortlessly personal. To get there, we focused on evolving the tech stack, refining the user experience, and embedding analytics at every step.
It all ties back to the aspect of habits. At the outset, we had limited visibility into how the app was being used, but we were able to see the key features that people use in our patient portal. We started with that to redesign the home screen and pull those features forward. We built in the analytics to track that, and from there, we could better understand patient behavior and iterate based on those insights.
Each time we iterated, we built in more analytics to go deeper into the journey. We could understand a little bit more, like an experiment on pulling forward appointment details as a key thing to show on the home screen. We improved navigation to surface key patient needs and built in tracking to validate our assumptions. It gave us a live feedback loop that continues to inform our strategy today.
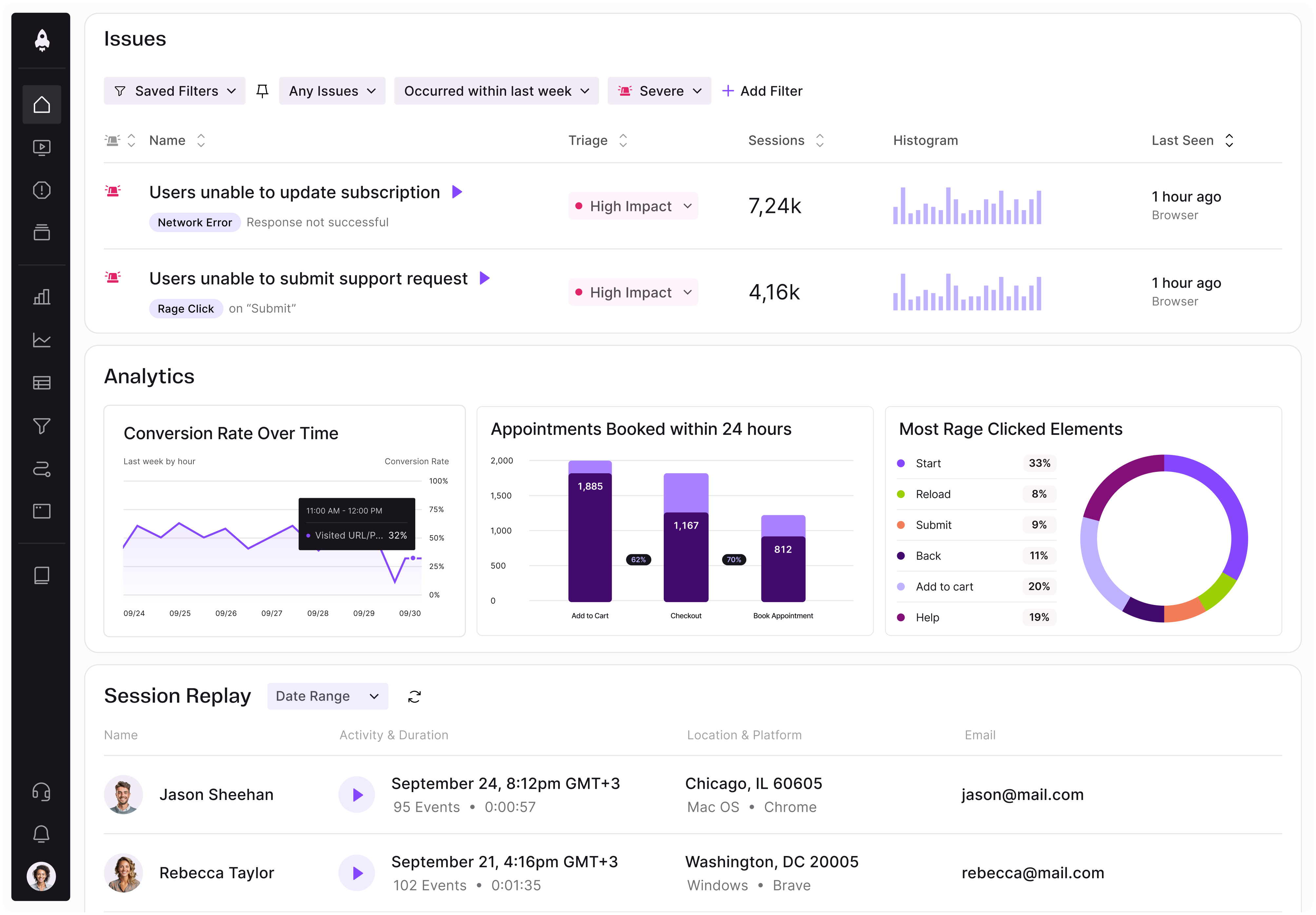
LogRocket identifies friction points in the user experience so you can make informed decisions about product and design changes that must happen to hit your goals.
With LogRocket, you can understand the scope of the issues affecting your product and prioritize the changes that need to be made. LogRocket simplifies workflows by allowing Engineering, Product, UX, and Design teams to work from the same data as you, eliminating any confusion about what needs to be done.
Get your teams on the same page — try LogRocket today.

Maryam Ashoori, VP of Product and Engineering at IBM’s Watsonx platform, talks about the messy reality of enterprise AI deployment.
A product manager’s guide to deciding when automation is enough, when AI adds value, and how to make the tradeoffs intentionally.

How AI reshaped product management in 2025 and what PMs must rethink in 2026 to stay effective in a rapidly changing product landscape.

Deepika Manglani, VP of Product at the LA Times, talks about how she’s bringing the 140-year-old institution into the future.